

Allegiance Benefit Plan Management, Inc. (Allegiance) is very proud to provide claims processing services
to the Collier County Board of County Commissioners. We have a dedicated service team and will provide you
with excellent service. An onsite Allegiance representative will be placed in the Risk Management office to
assist members with claims issues.
The Collier County Board of County Commissioners, through its Risk Management Department, administers the
group health benefit program for the County Manager agency and participating Constitutional Officers. Member
communications will be coordination between the Risk Management Department and Allegiance.
The links above will allow you 24 hour access to a variety of information about your claims, enrollment, flex
account, HRA account and more.
To submit a question via email not addressed in the information contained in the links above, please click on
the link "Contact Us” and you will receive a list of ways to contact us. Expect a reply within one to three
business days.
Better Health Benefits
Start with Allegiance
Since 1981, the Allegiance Companies have earned a reputation for quality,
service, and efficiency unmatched throughout the country. Since its earliest days, our company has
been a leader in providing health benefit plans to employer groups and plan participants throughout
the United States.
We have always remained dedicated to one thing: outstanding customer service. That commitment continues today as strong as ever.
Our corporate spirit has always been one of allegiance to the companies we serve. Our people are deeply committed to our clients
and to plan participants.
Resources for Members
Videos
Please Note: The walkthrough video reflects general login instructions. Please continue to log in using the login link on this custom site.
Take Allegiance On the Go
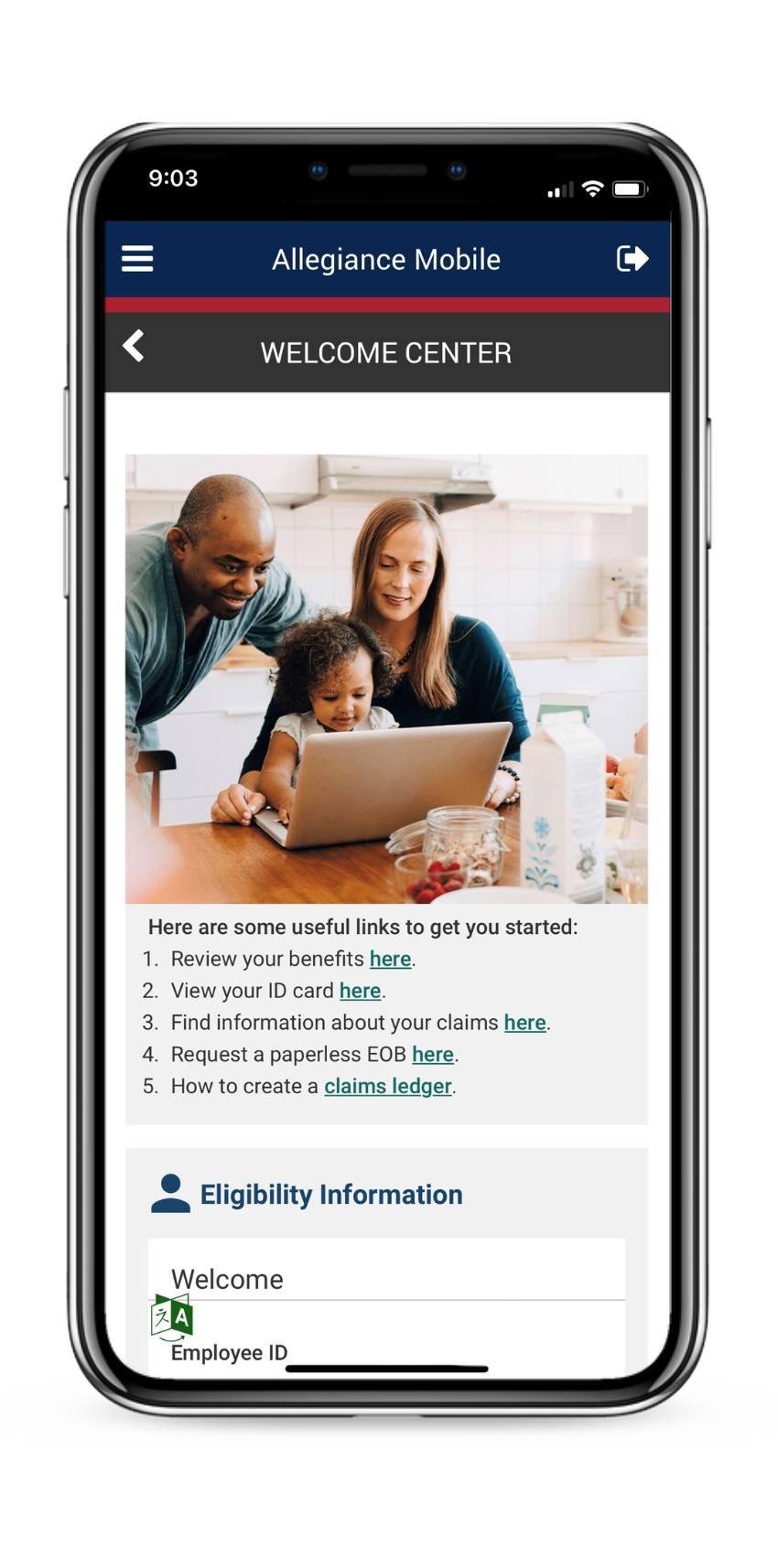
Our website offers personalized services at the click of a mouse. By registering, you will have 24
hour access to information regarding your health plan. You can check the status of a claim, review coverage
and benefits, and verify who is covered under your plan.
These services are also available through the Allegiance Mobile App available in Google Play and Apple App
stores.
Contact Us
2806 S. Garfield St.
P.O. Box 3018
Missoula, MT 59806
8:00 am - 4:00 pm EST
Customer Service 1-855-333-1004
Allegiance Holiday Closures
| New Year's Day | January 1st |
| Martin Luther King Jr. Day | Third Monday in January |
| President's Day | Third Monday in February |
| Memorial Day | Last Monday in May |
| Independence Day | July 4th |
| Labor Day | First Monday in September |
| Thanksgiving Day | Fourth Thursday in November |
| Friday after Thanksgiving | Fourth Friday in November |
| Christmas Eve | (1/2 day) December 24th |
| Christmas Day | December 25th |
Notice
For assistance regarding a claim or to pre-notify for medical services,
please call the customer service number at 1-855-333-1004.
CAA Customer Balance Billing Disclosure Out-of-Network

